Response mechanism of ICB among patients with breast cancer and novel approach to predicting therapeutic efficacy
Immunotherapeutic drugs, as represented by immune-checkpoint blockade (ICB), have achieved tremendous success in curing various tumors in recent years, thus improving the survival and life quality of some tumor patients in an appreciable manner. Recent data from clinical trials on breast cancer patients suggest that ICB, in combination with neo-adjuvant chemotherapy, can improve the pathological complete response (pCR) rate and the event-free survival rate in breast cancer. Neo-adjuvant ICB is expected to become part of the standard of care for breast cancer treatment. However, not all breast cancer patients respond to neo-adjuvant ICB. It is therefore essential to identify which underlying mechanisms and associated markers determine treatment response and develop new methods to predict the population who will benefit from neo-adjuvant therapy and practice precision medicine.
The findings, based on collaborative research by Prof. QIAN Junbin from Women’s Hospital affiliated to the Zhejiang University School of Medicine, Prof. Ann Smeets from the University Hospitals Leuven, KU Leuven and Prof. Diether Lambrechts from the VIB Center for Cancer Biology (Belgium), were published in an article entitled “A single-cell map of intratumoral changes during anti-PD1 treatment of patients with breast cancer” in the journal Nature Medicine. In their study, researchers conducted a window-of-opportunity trial involving patients with early-diagnosed breast cancer. Paired pre- versus on-treatment biopsies from treatment-naive patients receiving anti-PD1 (n = 29) or patients receiving neo-adjuvant chemotherapy before anti-PD1 (n = 11) were subjected to single-cell transcriptome (scRNA-seq), T cell receptor (scTCR-seq) and combined transcriptome and proteome (CITE-seq) profiling. By analyzing the variations of cell phenotypes in the tumor microenvironment before and after the immunotherapy, researchers identified specific types of cells that are potentially conducive to immunotherapeutic efficacy, in particular cell subtypes associated with T cell clonal expansion.
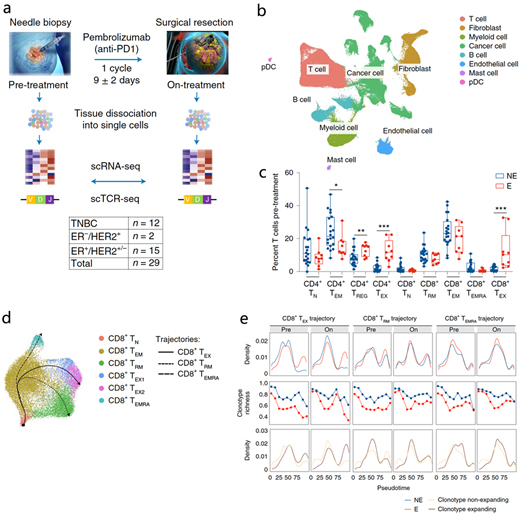
Research design and variations of cell phenotypes in the tumor microenvironment before and after immunotherapy
By comparing the immune microenvironments of patients with and without T cell clonal expansion, researchers discovered the differentiation pattern of cells from several immunophenotypes during immunotherapy and the possible mechanism. For example, this study suggested that several subtypes of CD4+ T cells and CD8+ T cells are target cells in anti-PD-1. Moreover, CD8+ TEX cells and CD4+ TEX cells, which could be separated into TH1 and TFH cells, lead to clonal expansion and are likely to contribute to ICB response. In pre-treatment biopsies, the relative frequency of immunoregulatory dendritic cells (PD-L1+), specific macrophage phenotypes (CCR2+ or MMP9+) and cancer cells exhibiting major histocompatibility complex class I/II expression correlated positively with T cell expansion. Conversely, undifferentiated pre-effector/memory T cells (TCF7+, GZMK+) or inhibitory macrophages (CX3CR1+, C3+) were inversely correlated with T cell expansion. These data identify various immunophenotypes and associated gene sets that are positively or negatively correlated with T cell expansion following anti-PD1 treatment.
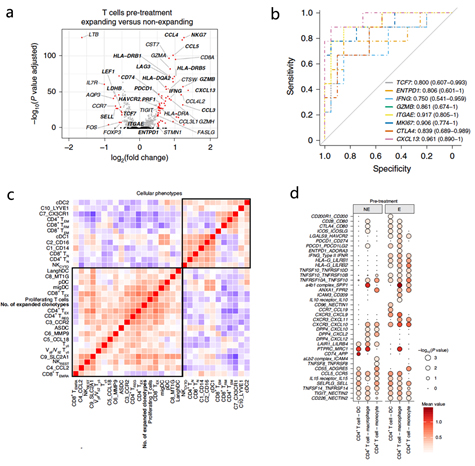
Immune microenvironments and biomarkers associated with immunotherapy response
“This study thus provides insights into potential predictive biomarkers of post-ICB clinical benefit,” said QIAN Junbin, adding that the research paradigm is expected to be applied to the study of other tumors and even other diseases.